Creating New Stem Cells
June 26, 2014
In places including the United States, the progress of research based on stem cells—the original unformed cells that differentiate to constitute all the body’s organs and tissues—has been slowed by ethical concerns about using human embryos as a source of the cells.
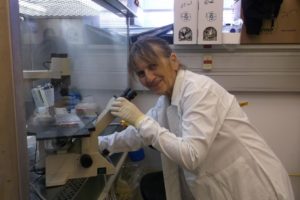
In 2012, a Japanese scientist, Shinya Yamanaka, won the Nobel Prize for creating induced pluripotent stem cells (iPSC): basic cells that can differentiate into various specialized cells. Dr. Rivki Ofir, a senior research associate at BGU’s Center for Regenerative Medicine, Cellular Therapy and Stem Cell Research, bases her work on this breakthrough and leads it in new directions.
“My main purpose is to reprogram patient cells into embryonic stem-like cells and then instruct them to become a cell related to a disease,” explains Dr. Ofir.
“These cells carry the patient’s genetic information and can become any of the body’s cell types. This is helpful as many cell types are not readily accessible from patients. IPSC cells, when turned into adult cell types, play out the disease in a manner similar to that of cells in the patient.”
For example, skin cells from a person with a congenital heart disease can be reprogrammed to become embryonic cells, and then instructed to become heart cells. These cells are used to model the disease in a Petri dish and are then comprehensively studied to find underlying causes.
Patients, hoping a family disease can be remedied, are happy to provide samples, Ofir says. “We follow the protocol generated by Yamanaka and use a manipulation to bring the cells back to the embryonic state, the starting point of a human being when the egg and sperm are together.”
The process centers on introducing a particular kind of virus into the cells, but Ofir and her colleagues are experimenting with various chemicals to accomplish the goal.
To date, what she finds most exciting is seeing the heart cells she created.
“We started the whole process from nothing—took skin cells, reprogrammed them to behave like stem cells, and then used the protocol to instruct them to become heart cells. We can see them beating in the Petri dish!”
Studying the genes that are responsible for a disease in a Petri dish helps researchers figure out how the mutation dictates the defect and enables them to look for a new drug remedy. Investigating monogenic diseases, common to the Bedouin, can lead scientists to extrapolate that understanding to the mechanism of diseases like ALS, where the specific mutation is not known.
“It may seem like no big deal to study a unique disease in an isolated tribe in the desert,” Ofir explains, “but you may learn something that can be important to the general population if there’s a similarity between the diseases.
“Doing regenerative medicine in a dish can teach us about dimensions and structure. You learn about the signals required for the organism to survive. And we work for our second goal: to use the cells for drug discovery. Using human cells offers many advantages.
“For example, when you use mice for clinical studies with a heart drug, there are big problems because a mouse’s heart is different from a human’s. A drug might be good for mice, but kill people. So we try to model the disease in the reprogrammed human cells for better preclinical studies.”
Ultimately this disease-in-a-Petri dish approach may empower scientists to “correct” genetically defective heart cells, and then transplant them into that person’s body to make new heart muscle. A major benefit of this procedure is that it would not trigger the auto-immune responses that often lead the body to reject a transplant.
“But much needs to be learned,” Ofir says.
Her own contribution is to create as many disease models as she can to support the study of neurological, muscular, metabolic, musco-skeletal diseases, and more.
“I dream of a freezer full of fibroblasts, skin or blood cells from many different patients, which we can then reprogram to produce pluripotent stem cells. Then we can start to learn how the mutated gene leads to the disease. That’s my mission!”
The work could not be done without the new Center, Ofir states.
“We couldn’t ask these questions on the level of the stem cell before, and understand why the disease happens. The new methods will help us make huge progress in understanding the causes and looking for potential cures.”
In addition to creating heart cells, researchers are making great strides in producing pancreatic cells, and Ofir is excited about working with epilepsy. She is also looking toward collaborating with other Center scientists on Alzheimer’s research.