A Robotic Oasis in the Negev
May 10, 2017
This is an excerpt from an article by Maayan Jaffe-Hoffman appearing in the May 15, 2017 issue of The Jerusalem Report.
The Jerusalem Report — Israel’s Negev desert appears to be the opposite of futuristic. But within that desert there is an oasis of technology that facilitates robotics envied by the world.
In each of several laboratories at Ben-Gurion University, humans and robots interact, working hand in hand in an effort to solve medical problems previously thought impenetrable.
“You name it, and we are working on it,” says Prof. Hugo Guterman, head of BGU’s Laboratory for Autonomous Robots.
Prof. Guterman says he got into robotics “by mistake.” But there are two reasons he sticks with it: “One is the possibility that we can improve how things we used to accept as ‘Mother Nature’ are really done,” he says.
“The second is that you can solve problems and actually help people.”
An example of this is Prof. Amir Shapiro’s Balance Tutor. Invented with Prof. Itzik Melzer, head of the Leon and Matilda Recanati School for Community Health Professions, the Balance Tutor measures the level of balance in elderly people and trains them to balance better.
It is the only rehabilitation system that employs an advanced 4D perturbation patented treadmill, multiple force and movement sensors and customized motivational video games. The technology was licensed to Netanya-based MediTouch and is now sold to physical therapy clinics around the world.
BGU and Cincinnati Children’s Hospital combined efforts to launch Xact Medical and bring to market the Fast Intelligent Needle Delivery (FIND) system, which uses robotics and ultrasound to better guide and insert a needle into a patient’s body.
“It is very common to make mistakes when trying to introduce a needle into a vein,” says Prof. Guterman, who worked on the project. “There is only about a 70 percent first-try success rate and as many as 300 people die per year in the United States from complications of misplaced needles.”
FIND puts the needle and the ultrasound into a singular robot, which both identifies the best location to insert the needle and automatically inserts it. The whole process takes less than 30 seconds. Prof. Guterman’s team is now working on expanding the use of this technology for other medical uses, including biopsy, chemotherapy and the administration of intravenous drugs.
Another one of Prof. Guterman’s projects centers on physical therapy (PT). Patients in need of care have to wait too long to get appointments and are charged with doing PT exercise at home without any feedback from their therapist. Therefore, many people fail to do the required exercises, delaying or inhibiting recovery.
“Now, suppose you were able to do those exercises in your house, but you had a system that continuously transferred information from you to your therapist in real time?” asks Prof. Guterman.
“What if your therapist could respond and change your program in reaction to how you are doing? This would improve the quality of service and reduce the time until recovery.” Prof. Guterman’s lab is determining the best way to leverage existing technology to make such a system work.
Prof. David Zarrouk, of BGU’s Department of Mechanical Engineering and head of the University’s Bio-Inspired and Medical Robotics Lab, is working on a self-propelled camera capsule that will assist doctors in seeing the small intestine.
The patient will swallow the tiny robotic device, which will work its way through the digestive system. But rather than passively moving through the body, Prof. Zarrouk’s capsule will be controlled by the doctor.
“The doctor will be able to halt the device and get a more optimized view,” says Prof. Zarrouk.
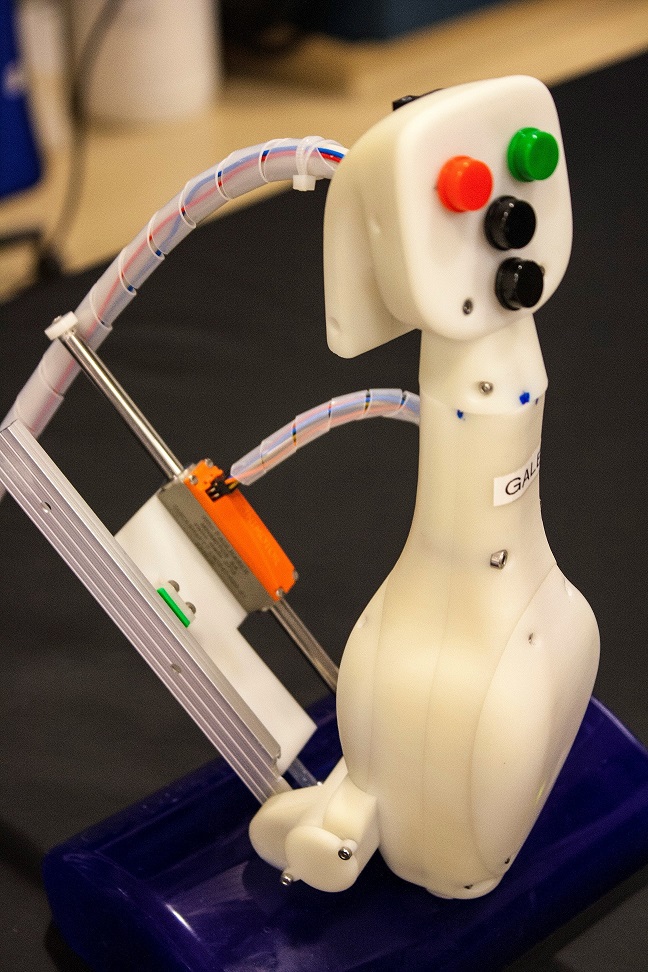
Prof. Shapiro is working on improving the functioning of robotic hands – not the kinds humans use if they are born without a hand or lose one in an accident, but the hands of robots themselves. Currently, most robots have very simple grippers at the end of their arms that are used to grasp specific objects. Prof. Shapiro is hoping to design a hand that will allow the robot to better manipulate its hand movements and grasp more detailed and diverse items.
From a medical standpoint, this could mean grasping internal organs for a doctor during surgery or holding the stomach during a sleeve gastrectomy, surgery conducted for weight loss.
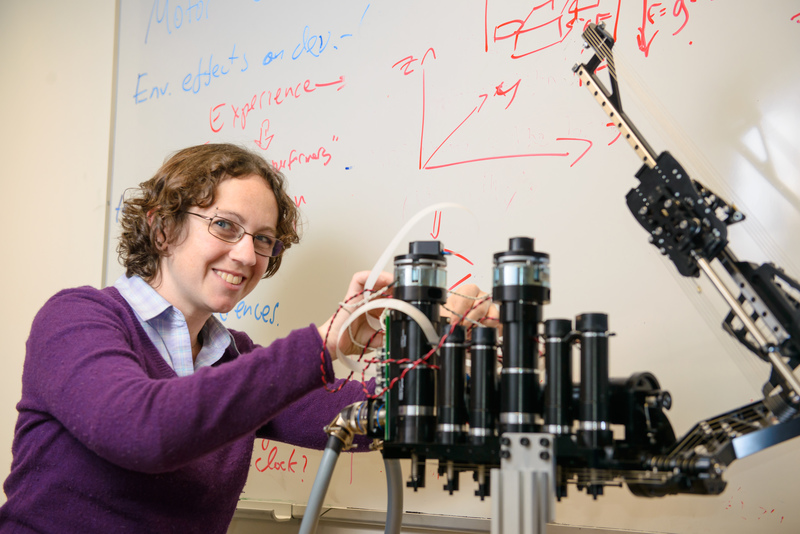
Dr. Ilana Nisky, of BGU’s Biomedical Robotics Lab, is using robots, haptic devices and other mechatronic devices as a platform to understand the human sensorimotor system in real-life tasks like surgery.
Practically, she is trying to understand “how our brain succeeds in controlling the motions of our hands and how we process information that we acquire through our sense of touch,” she says. Her goal is to design software that will give surgeons conducting robot-assisted procedures physical information about what they are touching and how they are touching it.
There are multiple advantages to such software. For starters, it will improve the time needed for surgeons to become experienced robotic surgeons. It will also make conducting minimally invasive surgeries easier.
“During standard laparoscopic surgery, the surgeon needs to work with long instruments that impose strong challenges on their motor system,” says Dr. Nisky. “With robotic surgery you gain a more natural motion and more freedom, plus you get better 3D visualization, but you still cannot feel what you are doing.” Her software would change that.
What’s more, Dr. Nisky says that as robotic surgery advances, there is no reason why the surgeon and patient would need to be in the same location, because the surgeon would simply be manipulating a robot through an external device.
Despite rapid advances, Prof. Guterman says there are various bureaucratic, economic and ethical barriers for robotic devices to enter the marketplace. It costs a lot to do clinical trials, and the time it takes to get medical devices FDA approved can be anywhere from six months to several years.
There is also a fear among some doctors that robotics will put them out of work, but Prof. Guterman does not share this fear.
“Robots cannot replace doctors because there is a lot of know-how that is not well defined,” he says. “In many cases, doctors treat not solely based on the knowledge they get from a textbook, but based on information they receive from conversations with patients.”
“I think doctors will ultimately prefer to have free time to talk with patients, rather than wasting their time making cuts or doing procedures that could just as well be done by a machine,” Prof. Guterman explains.
“We don’t know what is in the future for us, but the bottom line is that society has much to gain from medical robots.”